Abstract
BACKGROUND Lymphoma is a malignancy of the lymphatic system that arises from clonal proliferation of B-cells, T-cells, or natural killer cells. It is one of the most common malignancies in adults, with an incidence of approximately 82,000 new cases annually in the United States (Lewis et al., 2020).
Over the past decade, immunotherapy has become increasingly important in lymphoma treatment. Rituximab was the first monoclonal antibody approved for oncological care and has become the gold-standard for management of B-cell malignancies. Over the years, checkpoint inhibitors, drug-antibody conjugates, bispecific antibodies, and chimeric antigen receptor T (CAR T) cell therapy have also been incorporated into guidelines of standard care.
The first CAR T therapy for the treatment of diffuse large B-cell lymphoma was FDA approved in October 2017. Approval for follicular, mantle cell, and other types of lymphoma soon followed.
Outpatient administration of immunotherapy has become progressively more frequent due to the convenience and associated lower costs. However CAR T therapy is still largely administered inpatient, as institutions hesitate to transition to an outpatient setting due to logistical barriers and concerns for toxicity (Myers et al., 2021).
This study evaluates trends and outcomes of hospitalizations for immunotherapy in patients with lymphoma over a decade.
METHODS Using the National Inpatient Sample (NIS) database from 2010 to 2019, we identified adult patients with immunotherapy as the primary reason for admission and those who also had a secondary diagnosis of lymphoma using ICD-9 and ICD-10 codes. Trends for in-hospital mortality, total hospital charges, and length of hospital stay were evaluated. Multivariate logistic regression analysis was conducted to adjust for confounders. J-point analysis was used to assess statistical significance of incidence trends.
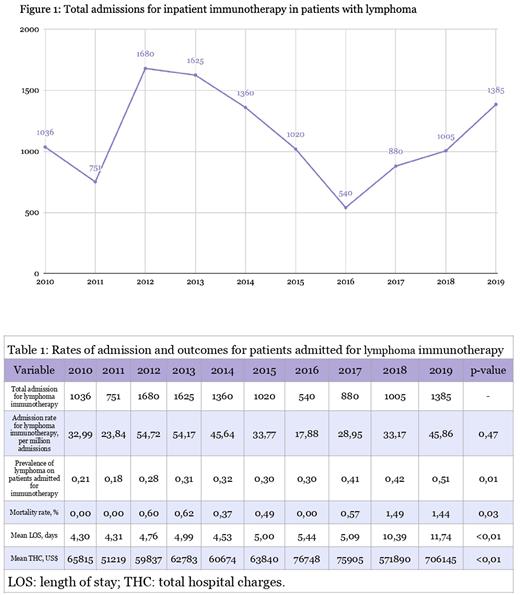
RESULTS From 2012 to 2016 there was a gradual decrease in the total number of admissions for immunotherapy for lymphoma (Figure 1). However, starting in 2017 there was a reversal of this trend, and the number of admissions started increasing.
By 2019, the proportion of patients with lymphoma admitted for immunotherapy, compared to that of all other cancers, increased to 51% from 21% in 2010 (p<0.01, Table 1). Additionally, there was a statistically significant increase in the mean length of stay, from 4.3 to 11.7 days (p < 0.01), and total charges for admissions increased from $65,815 in 2010 to $706,145 in 2019 (p < 0.01).
CONCLUSIONS Our study showed an increase in the number of immunotherapy admissions for lymphoma starting in 2017, which coincides with the introduction of CAR T therapy for this subset of cancers. In 2019, lymphoma became the most frequent malignancy in patients receiving inpatient immunotherapy. Over the period studied, there was a 2.7-fold increase in the length of stay and a ten-fold increase in total charges.
Although inpatient administration of checkpoint inhibitors and bispecific antibodies might be contributing to the trend, these therapies are significantly less costly than CAR T therapy. We speculate the significant increase in charges and length of stay primarily represents the impact of the introduction of CAR T-cells for the therapy of lymphomas. Further studies are needed to better characterize the economic burden and systemic impact of inpatient administration of CAR T therapy and other immunotherapies in the treatment of lymphomas.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.